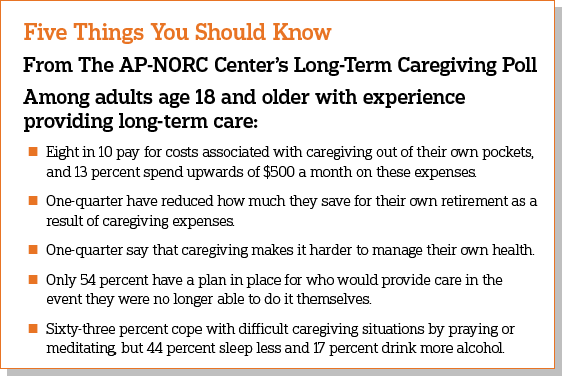
As family and friends take on more of the responsibility of caring for the nation’s growing senior population, their own personal and professional lives often pay the price, according to a new study from The Associated Press-NORC Center for Public Affairs Research. For about one-quarter of America’s informal caregivers, the amount of time they spend providing care each week is the equivalent of a full-time job. Beyond the hours they spend caregiving, 8 in 10 pay for caregiving costs out of their own pockets, with 13 percent spending $500 or more a month. For the majority of caregivers with incomes of less than $50,000, these costs impose a significant burden. Forty-three percent of these caregivers have dipped into their personal savings, and 23 percent have reduced how much they save for their own retirement, suggesting that the financial impacts of informal caregiving are significant and long lasting.
Many who take on a caregiving role face significant health challenges themselves. Fully 39 percent of caregivers have a health condition, physical limitation, or mental health condition that affects their daily life or limits their own activities, and 40 percent of this group say that providing care makes it harder to manage their own health. In addition, a majority of caregivers report having less free time or less time for socializing with friends, and nearly half of caregivers who work have used their vacation time to provide care.
Despite these challenges, a majority of informal caregivers view their role as an important if not essential part of their personal identity, and most find healthy ways to cope with the stresses of providing long-term care. Sixty-three percent pray or meditate, and 51 percent spend time outside. However, some caregivers employ such unhealthy behaviors as sleeping less (44 percent), avoiding talking to people about the situation (38 percent), drinking more alcohol (17 percent), or smoking or using tobacco more (17 percent).
More than half of current caregivers feel lonely at least some of the time. Age is a strong factor in these feelings. Those age 18-39 are much more likely to report feeling lonely compared to caregivers age 40 and older (74 percent vs. 46 percent). This age difference is in line with a prior AP-NORC poll finding that, although those under 40 spend less time providing care, they are more likely than older caregivers to report being stressed by caregiving.
Since 2013, The AP-NORC Center has conducted annual surveys investigating older Americans’ experiences and attitudes regarding long-term care to contribute data to help policymakers, health care systems, and families address this issue. Prior years of the poll focused on Americans age 40 and older. For the first time, this year’s study also explored the perspectives of younger adults, those age 18-39, generating new insights into their personal experiences with caregiving and their views of long‑term care. This survey from The AP-NORC Center dives further into the experiences of informal caregivers age 18 and older, exploring the opportunity costs and health impacts on those who devote their time to providing long-term care.
This AP-NORC Center study, with funding from The SCAN Foundation, includes 1,024 interviews with a nationally representative sample of Americans age 18 and older with past or current experience providing long-term care to a family member or friend. Forty-eight percent of the sample are current caregivers. Data were collected using NORC’s AmeriSpeak® Panel.